Mount Sinai is one of the oldest integrated healthcare systems in the U.S., with 7 hospitals, 1 medical school, 15 institutes, and over 40,000 employees, physicians, and residents.
Like other healthcare systems, Mount Sinai is impacted by a number of disruptive factors––from increasing demand for services because of aging populations to declining funds due to compressed budgets.
To address these challenges, Mount Sinai has prioritized preventive care – working with patients to proactively address the root causes of diseases like diabetes instead of only intervening after the disease occurs. This provides better care for patients, and reduces costs for the healthcare system. To achieve this type of proactive care, however, Mount Sinai needed a better way to share health data with its doctors, and its community care partners.
Challenge: Setting up a Single View of the Patient
Mount Sinai employs tens of thousands of physicians, caring for a total of 2.6 million inpatient and outpatients annually. However, whenever a doctor saw a patient, they had to look through an average of 5 applications to get a comprehensive view of the patient’s medical record.
The number of siloed data sources challenged efforts to improve the patient experience and streamline how doctors provide care, demanding a new approach to connectivity.
Challenge: Sharing Data with Community Care Providers
Mount Sinai partners with community partners, such as the Salvation Army, to support community care initiatives. These partners had no visibility into a patient’s medical record. This caused medical information to slip through the cracks and prevented caseworkers from effectively coordinating with Mount Sinai to provide better care to the patient.
As a result of the lack of integration between disparate sources of data, Mount Sinai was unable to achieve a single view of the patient or enable partners by sharing relevant data with them. This is because it would take Mount Sinai months to give a new application access to important data––preventing them from taking advantage of the latest technology in a way that would help them create a single patient view, partner with community care providers, and improve care.
Solution: Breaking Down Data Silos to Build a Single Patient View and Improve Partner Collaboration
To address the lack of data interoperability, Mount Sinai turned to their IT team to transform care by building a single patient view and improving coordination between physicians, caseworkers, and community care providers. This required breaking the silos between the medical and non-medical data, applications, systems, and devices used by Mount Sinai teams and community partners.
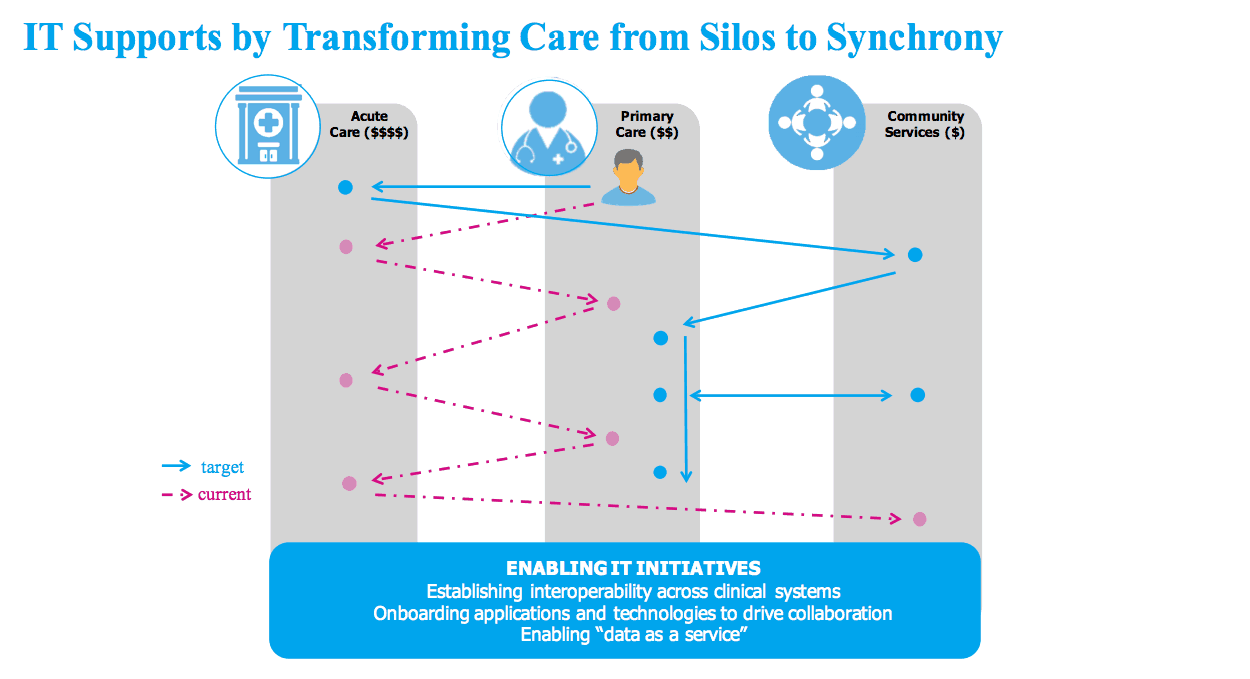
Using MuleSoft, Mount Sinai was able to bring together siloed data in a variety of applications and systems – from medical systems to billing applications – and build a single patient view using API-led connectivity, an approach in which applications, data, and devices are exposed as APIs.
Before Mount Sinai integrated these data sources, patients might not seek out care unless their conditions were so severe that they required an ER visit. This leads to a worse outcome for the patient, and higher costs for Mount Sinai. By bringing together siloed data and establishing better collaboration with community care providers, Mount Sinai can now promote preventive care practices, reduce ER re-admissions, and, in turn, improve care and lower costs.
How? With Anypoint Platform, Mount Sinai exposed data from systems and applications through Fast Healthcare Interoperability Resources (FHIR) APIs. The hospital system can now share data through these APIs with hundreds of community care organizations and healthcare providers across New York City; thereby improving collaboration.
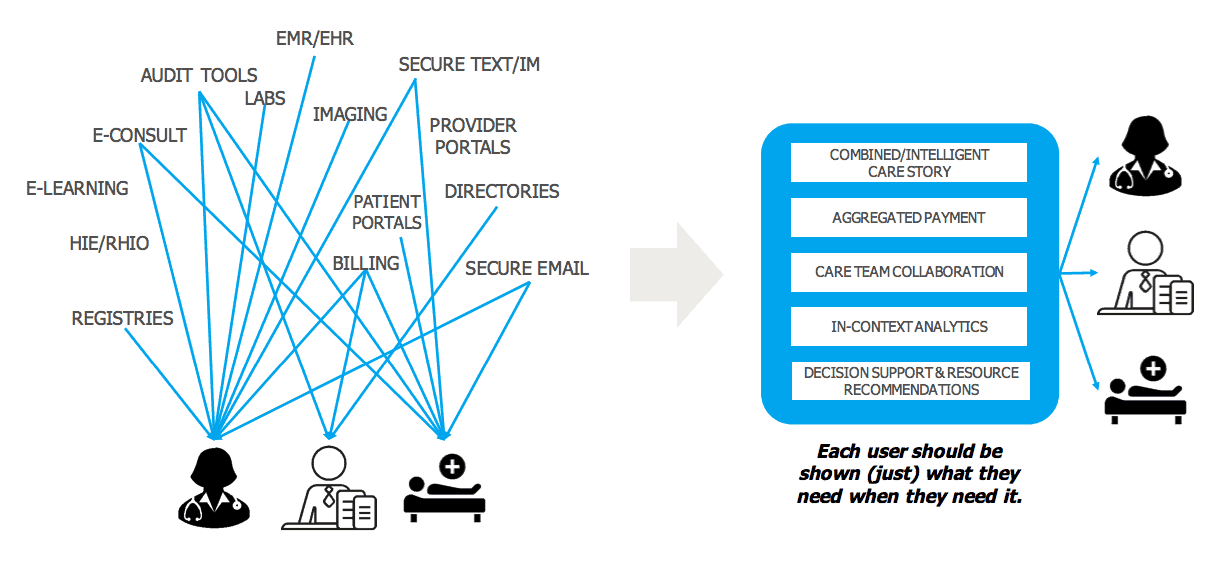
With API-led connectivity and MuleSoft’s library of pre-built connectors for systems like Salesforce, Mount Sinai has been able to easily surface Electronic Health Record (EHR) data across both clinical and non-clinical applications. This means that care providers now have real-time, unified visibility to patients’ medical histories, medication records, lab results, and past treatments either on the desktop computers in their office or on their mobile phones.
Mount Sinai can now ensure that not only is this visibility available to care providers, but community partners and caseworkers also have similar visibility into each patient’s healthcare journey. For example, the Salvation Army can now use the available data to identify diabetes patients who need reminders to take their medication. Doctors and community partners can now work as a single care team to drive best-in-class care outside the four walls of the hospital.
For Mount Sinai, a single patient view is no longer a goal – but a reality.
Take a look at more resources to see how API-led connectivity can drive healthcare innovation in your organization.
All illustrations are taken from Mount Sinai’s Summit Presentation.